Meet the Implementation Science Teams
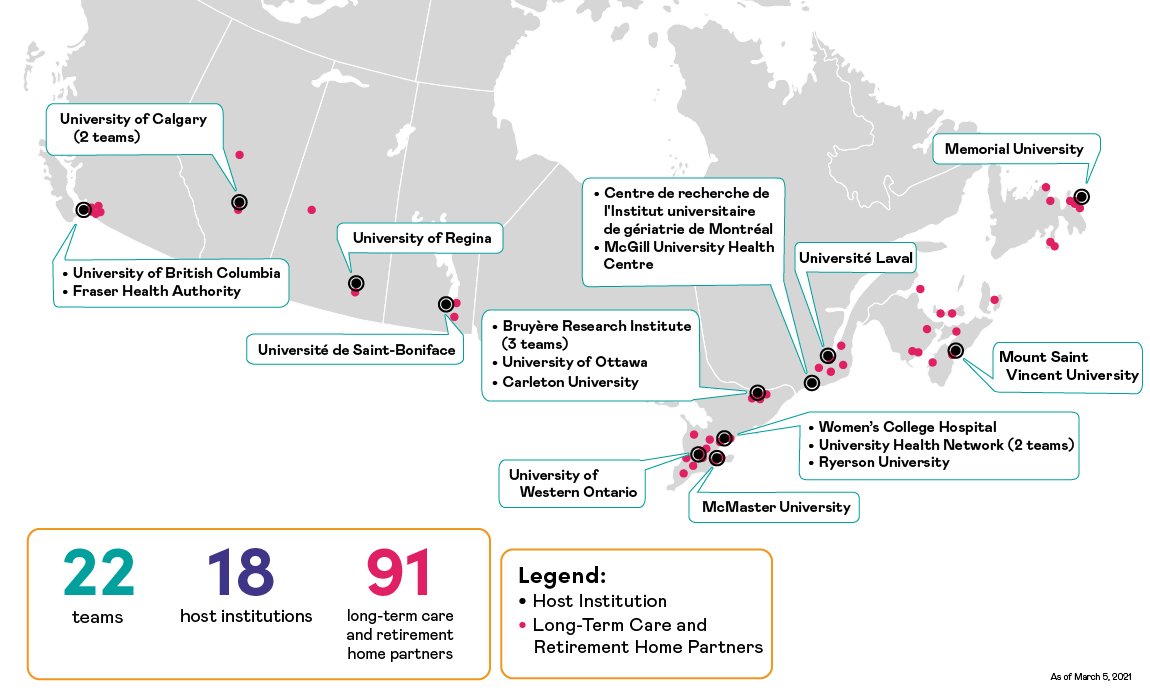
Twenty-two Implementation Science Teams of researchers from across the country have partnered with LTC and retirement homes, including homes that are part of the LTC+ Acting on Pandemic Learning Together program, to study the effectiveness of promising practices, interventions and policy options designed to keep residents, families, caregivers and staff safe from COVID-19.
In this section :
-
Implementation Science Teams – Strengthening Pandemic Preparedness in Long-Term Care
- Meet the Implementation Science Teams
Presence of family: (re)integrating family caregivers
Lead researcher: James Conklin
Host institution: Bruyère Research Institute, Ontario
Presence of family: (re)integrating family caregiversLead researcher: James Conklin |
|
Presence of family: (re)integrating family caregivers
Promising practice: Presence of family
Jurisdictions of focus: Ottawa, Markdale, Tavistock (Ontario)
The objective of this study was to allow essential care partners, who are chosen by the resident and who provide them with vital physical/psycho-social care, to have safe access to the long-term care home during and after the current pandemic.
The Designated Care Partner program in the three participating long-term care homes was strongly supported by residents, families, and staff, and is believed to have resulted in improved health and well-being for residents of the homes. Overall, findings show that the care provided by care partners is essential. Numerous people who provided data told the research team that care partners play two roles in long-term care: they care for the resident and they advocate on behalf of the resident. The research team also heard from many long-term care leaders and team members who indicated that they witnessed first-hand the importance of the role played by care partners and the need to bolster the staff-family relationship to ensure staff and care partners are working in harmony and pursuing a joint goal.
This research identified the following principles for improving long-term care in Ontario (where this research project was based):
- Reduce reliance on compliance: Invest in care staff to ensure residents are always able to receive care.
- Collaborate with residents, family, friends and staff: Engageto identify and share ideas and to work together to design and implement improvements.
- Empower long-term care homes and key stakeholders: All long-term care homes are unique and each home should be empowered to design and implement solutions that work best for their home.
- Learn together as we work our way toward a better world for older adults: Improvement efforts in long-term care should adopt a social learning process, bringing stakeholders from long-term care homes across jurisdictions to share experiences and to help each other move their improvement plans forward
Resources:
Presence of family: (re)integrating family caregiversLead researcher: James Conklin |
|
Promising practice: Presence of family The objective of this study was to allow essential care partners, who are chosen by the resident and who provide them with vital physical/psycho-social care, to have safe access to the long-term care home during and after the current pandemic. The Designated Care Partner program in the three participating long-term care homes was strongly supported by residents, families, and staff, and is believed to have resulted in improved health and well-being for residents of the homes. Overall, findings show that the care provided by care partners is essential. Numerous people who provided data told the research team that care partners play two roles in long-term care: they care for the resident and they advocate on behalf of the resident. The research team also heard from many long-term care leaders and team members who indicated that they witnessed first-hand the importance of the role played by care partners and the need to bolster the staff-family relationship to ensure staff and care partners are working in harmony and pursuing a joint goal. This research identified the following principles for improving long-term care in Ontario (where this research project was based):
Resources: |
RESPECT–LTC
Lead researcher: Amy Hsu
Host institution: Bruyère Research Institute, Ontario
RESPECT–LTCLead researcher: Amy Hsu |
|
RESPECT–LTC
Promising practice: Plan for COVID-19 and non-COVID-19 care
Jurisdictions of focus: Ottawa, Brampton (Ontario)
For long-term care (LTC) residents with and without COVID-19, palliative approaches to care are vital for quality care. However, the capacity of LTC homes to introduce and embed palliative care can be hindered by poor communication or information about prognosis.
In our project we will rapidly implement and evaluate the Risk Evaluation for Support: Predictions for Elder-life in the Community Tool in LTC (RESPECT–LTC), to support health and social service providers’ ongoing efforts to embed palliative approaches to care in their processes and culture.
RESPECT–LTC is a mortality-risk communication tool that accurately predicts an older adults’s six-month mortality risk as well as life expectancy, to inform health and social service providers’ decision-making regarding the initiation of palliative and/or end-of-life care. The tool was co-designed with patients and caregivers.
RESPECT–LTCLead researcher: Amy Hsu |
|
Promising practice: Plan for COVID-19 and non-COVID-19 care For long-term care (LTC) residents with and without COVID-19, palliative approaches to care are vital for quality care. However, the capacity of LTC homes to introduce and embed palliative care can be hindered by poor communication or information about prognosis. In our project we will rapidly implement and evaluate the Risk Evaluation for Support: Predictions for Elder-life in the Community Tool in LTC (RESPECT–LTC), to support health and social service providers’ ongoing efforts to embed palliative approaches to care in their processes and culture. RESPECT–LTC is a mortality-risk communication tool that accurately predicts an older adults’s six-month mortality risk as well as life expectancy, to inform health and social service providers’ decision-making regarding the initiation of palliative and/or end-of-life care. The tool was co-designed with patients and caregivers. |
Improving prescribing of medications at end of life in long-term care homes during COVID-19
Lead researcher: Peter Tanusepturo
Host institution: Bruyère Research Institute, Ontario
Improving prescribing of medications at end of life in long-term care homes during COVID-19Lead researcher: Peter Tanusepturo |
|
Improving prescribing of medications at end of life in long-term care homes during COVID-19
Promising practices: Preparation; plan for COVID-19 and non-COVID-19 care; people in the workforce
Jurisdictions of focus: Brampton (Ontario), Calgary (Alberta)
Partners: Ontario Palliative Care Network and Alberta Health Services
Palliative care is essential for long-term care (LTC) residents, whether or not they have COVID-19, with an average stay of 18 months and 25 percent dying in the first year after admission. Symptom management at end-of-life is essential to provide a comfortable death and is an excellent surrogate marker for palliative care delivery.
LTC providers may not have the expertise and/or time – especially with COVID-19 restrictions/pressures – to prescribe such essential medications. Our study aims for system-wide improvement in end-of-life care by:
- creating a new Quality Indicator for palliative/end-of-life care across all LTC homes
- improving staff through educational and other interventions
- improving pandemic response by improving low prescribers’ capacity to deal with deaths in subsequent waves of the pandemic
- improving planning for COVID-19 and non-COVID 19 care.
Improving prescribing of medications at end of life in long-term care homes during COVID-19Lead researcher: Peter Tanusepturo |
|
Promising practices: Preparation; plan for COVID-19 and non-COVID-19 care; people in the workforce Palliative care is essential for long-term care (LTC) residents, whether or not they have COVID-19, with an average stay of 18 months and 25 percent dying in the first year after admission. Symptom management at end-of-life is essential to provide a comfortable death and is an excellent surrogate marker for palliative care delivery. LTC providers may not have the expertise and/or time – especially with COVID-19 restrictions/pressures – to prescribe such essential medications. Our study aims for system-wide improvement in end-of-life care by:
|
Design Interventions to Support Infection Prevention and Control in Shared Work Environments in Long-Term Care
Lead researcher: Chantal Trudel
Host institution: Carleton University, Ontario
Design Interventions to Support Infection Prevention and Control in Shared Work Environments in Long-Term CareLead researcher: Chantal Trudel |
|
Design Interventions to Support Infection Prevention and Control in Shared Work Environments in Long-Term Care
Promising practice: Prevention and people in the workforce
Jurisdiction of focus: Ottawa, London (Ontario)
This project focused on the impact of design on the ability of staff to physically distance in their work environment. The research team identified key areas of congestion and crowding in two long-term care homes where they could rethink the design of the homes to reduce crowding.
Through extensive naturalistic observation, they were able to readily identify high traffic areas related to the design of the environment and associated products being used in the design. They were also able to identify aspects of the physical environment that influenced compliance with mask use. They are now working with the homes to implement a real-time location system to further validate these findings using quantitative data. They have also conducted preliminary design studies to remediate aspects of the environment contributing to crowding and mask use.
This study identifies risk factors in the design of the environment contributing to crowding and mask use. These findings provide evidence for rethinking the design of staff work areas to prepare homes for future outbreaks related to crowding and mask use.
Design Interventions to Support Infection Prevention and Control in Shared Work Environments in Long-Term CareLead researcher: Chantal Trudel |
|
Promising practice: Prevention and people in the workforce Jurisdiction of focus: Ottawa, London (Ontario) This project focused on the impact of design on the ability of staff to physically distance in their work environment. The research team identified key areas of congestion and crowding in two long-term care homes where they could rethink the design of the homes to reduce crowding. Through extensive naturalistic observation, they were able to readily identify high traffic areas related to the design of the environment and associated products being used in the design. They were also able to identify aspects of the physical environment that influenced compliance with mask use. They are now working with the homes to implement a real-time location system to further validate these findings using quantitative data. They have also conducted preliminary design studies to remediate aspects of the environment contributing to crowding and mask use. This study identifies risk factors in the design of the environment contributing to crowding and mask use. These findings provide evidence for rethinking the design of staff work areas to prepare homes for future outbreaks related to crowding and mask use. |
Nutrition as Medication: de la recherche à l’implantation
Lead researcher: Nancy Presse
Host institution: Centre de recherche de l'Institut universitaire de gériatrie de Montréal, Quebec
Nutrition as Medication: de la recherche à l’implantationLead researcher: Nancy Presse |
|
Nutrition as Medication: de la recherche à l’implantation
Promising practice: Plan for COVID-19 and non-COVID-19 care
Jurisdiction of focus: Montreal (Quebec)
Malnourishment and weight loss are endemic in long-term care (LTC) homes, and exacerbated during the COVID-19 pandemic. Since 2017, our team has been developing and testing a strategy called Nutrition as Medication (NAM) – prescribing small doses of an oral nutritional supplement, administered as medication in LTC homes. Preliminary results show NAM to be a promising approach to limiting, and potentially preventing, the decline in residents’ nutritional state, whether they have COVID-19 or not.
To equip LTC homes to better weather the pandemic, we are overseeing a large-scale adoption of NAM in LTC homes. We will evaluate its implementation, identify enabling and constraining factors, collect the opinions of LTC workers and caregivers/residents of the effect of NAM, and revise the NAM implementation in the context of the pandemic.
Nutrition as Medication: de la recherche à l’implantationLead researcher: Nancy Presse |
|
Promising practice: Plan for COVID-19 and non-COVID-19 care Malnourishment and weight loss are endemic in long-term care (LTC) homes, and exacerbated during the COVID-19 pandemic. Since 2017, our team has been developing and testing a strategy called Nutrition as Medication (NAM) – prescribing small doses of an oral nutritional supplement, administered as medication in LTC homes. Preliminary results show NAM to be a promising approach to limiting, and potentially preventing, the decline in residents’ nutritional state, whether they have COVID-19 or not. To equip LTC homes to better weather the pandemic, we are overseeing a large-scale adoption of NAM in LTC homes. We will evaluate its implementation, identify enabling and constraining factors, collect the opinions of LTC workers and caregivers/residents of the effect of NAM, and revise the NAM implementation in the context of the pandemic. |
A resident/family-centered, team-based quality improvement collaborative approach to comprehensive PAndemic Preparedness in LOng-term Care Homes (PAPLOC study)
Lead researcher: Akber Mithani
Host institution: Fraser Health Authority, British Columbia
A resident/family-centered, team-based quality improvement collaborative approach to comprehensive PAndemic Preparedness in LOng-term Care Homes (PAPLOC study)Lead researcher: Akber Mithani |
|
A resident/family-centered, team-based quality improvement collaborative approach to comprehensive PAndemic Preparedness in LOng-term Care Homes (PAPLOC study)
Promising practice: Preparation
Jurisdictions of focus: Abbotsford, New Westminster, Coquitlam (British Columbia)
To be effectively pandemic-prepared, long-term care (LTC) homes need rapid, comprehensive and customized implementation of promising practices and policies. Implementation can be supported through a systematic and collaborative approach to quality improvement (QI). COVID-19 restrictions mean that key QI partners, such as caregivers, care aides, nurses, healthcare professionals and managers/directors, often have to be engaged remotely.
In our study, we will use a virtual QI collaborative of LTC homes to investigate:
- Using Slack to facilitate a systematic QI approach to implement promising practices, to comprehensively address gaps in pandemic preparedness
- How this virtual collaboration tool can be used to scale-up and spread promising practices and policies for pandemic preparedness across multiple homes through a QI collaborative.
A resident/family-centered, team-based quality improvement collaborative approach to comprehensive PAndemic Preparedness in LOng-term Care Homes (PAPLOC study)Lead researcher: Akber Mithani |
|
Promising practice: Preparation To be effectively pandemic-prepared, long-term care (LTC) homes need rapid, comprehensive and customized implementation of promising practices and policies. Implementation can be supported through a systematic and collaborative approach to quality improvement (QI). COVID-19 restrictions mean that key QI partners, such as caregivers, care aides, nurses, healthcare professionals and managers/directors, often have to be engaged remotely. In our study, we will use a virtual QI collaborative of LTC homes to investigate:
|
Nurse practitioner-led implementation of health workforce recommendations in long-term care homes during a pandemic
Lead researcher: Katherine McGilton
Host institution: KITE, Toronto Rehabilitation Institute, University Health Network, Ontario
Nurse practitioner-led implementation of health workforce recommendations in long-term care homes during a pandemicLead researcher: Katherine McGilton |
|
Nurse practitioner-led implementation of health workforce recommendations in long-term care homes during a pandemic
Promising practice: People in the workforce and plan for COVID-19 and non-COVID-19 care
Jurisdiction of focus: Waterloo, Sarnia (Ontario)
This research aimed to develop and adapt a nurse practitioner (NP) led huddle intervention to the needs and context of two long-term care homes and to pilot test the huddle intervention and evaluate its implementation process and the influence of NP-led intervention on staff outcomes of moral distress, support, job satisfaction, and health.
A huddle implementation toolkit was developed through this work. Process evaluation revealed that it was feasible for NPs to implement huddles using the toolkit. Attendees of NP-led huddles reported less moral distress and perceived more support from the NP compared to non-attendees. Qualitative findings revealed factors strongly influencing huddle implementation in the long-term care context.
Nurse practitioners demonstrate themselves as leaders and supporters of the workforce and can successfully implement new practices. Huddles may be utilized to support the workforce of the long-term care sector and improve care. However, for successful implementation to occur, long-term care leaders must consider their involvement in huddles, the importance of including all team members in huddles to help build relationships and integrating NPs as full-time staff within long-term care.
Nurse practitioner-led implementation of health workforce recommendations in long-term care homes during a pandemicLead researcher: Katherine McGilton |
|
Promising practice: People in the workforce and plan for COVID-19 and non-COVID-19 care Jurisdiction of focus: Waterloo, Sarnia (Ontario) This research aimed to develop and adapt a nurse practitioner (NP) led huddle intervention to the needs and context of two long-term care homes and to pilot test the huddle intervention and evaluate its implementation process and the influence of NP-led intervention on staff outcomes of moral distress, support, job satisfaction, and health. A huddle implementation toolkit was developed through this work. Process evaluation revealed that it was feasible for NPs to implement huddles using the toolkit. Attendees of NP-led huddles reported less moral distress and perceived more support from the NP compared to non-attendees. Qualitative findings revealed factors strongly influencing huddle implementation in the long-term care context. Nurse practitioners demonstrate themselves as leaders and supporters of the workforce and can successfully implement new practices. Huddles may be utilized to support the workforce of the long-term care sector and improve care. However, for successful implementation to occur, long-term care leaders must consider their involvement in huddles, the importance of including all team members in huddles to help build relationships and integrating NPs as full-time staff within long-term care. |
MedSafer – Optimizing prescribing for pandemic preparedness
Leader researcher: Emily McDonald
Host institution: McGill University Health Center, Quebec
MedSafer – Optimizing prescribing for pandemic preparednessLeader researcher: Emily McDonald |
|
MedSafer – Optimizing prescribing for pandemic preparedness
Promising practice: Plan for COVID-19 and non-COVID-19 care
Jurisdiction of focus: Toronto, Ottawa (Ontario)
The objective of this study was to integrate MedSafer electronic decision support for deprescribing in long-term care in the Point Click Care electronic health record. The research team aimed to improve the process for medication management and test out a scalable deprescribing solution during the pandemic.
The research team was able to successfully integrate MedSafer in Point Click Care and demonstrate that electronic decision support is possible for deprescribing as a scalable solution. Given the pandemic context, they experienced some challenges including barriers to engaging with long-term care homes and staff and staff shortages contributing to limited uptake of MedSafer in one of the two long-term care homes they partnered with. The research team learned that there can be lots of competing challenges and often it can be difficult to make medication safety a number one priority.
The research team aims to make deprescribing a priority for medication reviews by generating interest in MedSafer and more specifically, how MedSafer can help facilitate medication management.
Resources
MedSafer – Optimizing prescribing for pandemic preparednessLeader researcher: Emily McDonald |
|
Promising practice: Plan for COVID-19 and non-COVID-19 care Jurisdiction of focus: Toronto, Ottawa (Ontario) The objective of this study was to integrate MedSafer electronic decision support for deprescribing in long-term care in the Point Click Care electronic health record. The research team aimed to improve the process for medication management and test out a scalable deprescribing solution during the pandemic. The research team was able to successfully integrate MedSafer in Point Click Care and demonstrate that electronic decision support is possible for deprescribing as a scalable solution. Given the pandemic context, they experienced some challenges including barriers to engaging with long-term care homes and staff and staff shortages contributing to limited uptake of MedSafer in one of the two long-term care homes they partnered with. The research team learned that there can be lots of competing challenges and often it can be difficult to make medication safety a number one priority. The research team aims to make deprescribing a priority for medication reviews by generating interest in MedSafer and more specifically, how MedSafer can help facilitate medication management. Resources |
Implementing and scaling up the long-term care palliative toolkit during COVID-19
Lead researcher: Sharon Kaasalainen
Host institution: McMaster University, Ontario
Implementing and scaling up the long-term care palliative toolkit during COVID-19Lead researcher: Sharon Kaasalainen |
|
Implementing and scaling up the long-term care palliative toolkit during COVID-19
Promising practices: Presence of family; preparation; people in the workforce; plan for COVID-19 and non-COVID-19 care
Jurisdictions of focus: Saint John (New Brunswick), Hamilton (Ontario), Battleford (Saskatchewan)
Long-term care (LTC) residents and families are often faced with making critical and emotional end-of-life decisions without any preparatory discussions, resulting in stress and conflict. We have developed a toolkit, Strengthening a Palliative Approach in LTC (SPA-LTC), to support the needs of residents, their loved ones and LTC homes.
SPA-LTC includes tools and practices to: engage residents and families across disease trajectories; develop workforce capacity through online education modules; reduce stress and improve psychological health; and develop organizational structures and processes to promote a palliative approach to care.
We will evaluate the toolkit’s implementation and effectiveness in LTC homes during COVID-19, assess scalability across the three provinces and identify ways to adapt the toolkit for diverse regions and contexts.
Implementing and scaling up the long-term care palliative toolkit during COVID-19Lead researcher: Sharon Kaasalainen |
|
Promising practices: Presence of family; preparation; people in the workforce; plan for COVID-19 and non-COVID-19 care Long-term care (LTC) residents and families are often faced with making critical and emotional end-of-life decisions without any preparatory discussions, resulting in stress and conflict. We have developed a toolkit, Strengthening a Palliative Approach in LTC (SPA-LTC), to support the needs of residents, their loved ones and LTC homes. SPA-LTC includes tools and practices to: engage residents and families across disease trajectories; develop workforce capacity through online education modules; reduce stress and improve psychological health; and develop organizational structures and processes to promote a palliative approach to care. We will evaluate the toolkit’s implementation and effectiveness in LTC homes during COVID-19, assess scalability across the three provinces and identify ways to adapt the toolkit for diverse regions and contexts. |
Enhancing the lives of older Canadians in long-term care in Newfoundland
Leader researcher: Shree Mulay
Host institution: Memorial University of Newfoundland, Newfoundland and Labrador
Enhancing the lives of older Canadians in long-term care in NewfoundlandLeader researcher: Shree Mulay |
|
Enhancing the lives of older Canadians in long-term care in Newfoundland
Promising practice: Presence of family
Jurisdictions of focus: Carbonear; St John’s; Placentia; Wabana, Bell Island; Clarenville; Bonavista; Grand Bank; St. Lawrence (Newfoundland and Labrador)
Our research focuses on long-term care (LTC) residents and family-centered care interventions – with the potential to change the way older adult care is provided in the province. Our aims include accelerating the availability of high-quality evidence to inform Canada’s rapid response to the COVID-19 pandemic; iterative testing to enhance local collaborative efforts and help reorient the existing research infrastructure; and providing evidence on older adults’ care for decision-making and planning throughout Canada.
The interventions will include: e-visits and electronic messaging; virtual mental health support; residents’ integrated COVID and non-COVID care plans including virtual care; and infection control and prevention training among LTC leadership.
Our findings will be relevant to all Canadian provinces with a population living in rural communities and small towns, and other settings that have similarities to those LTC homes in this province.
Enhancing the lives of older Canadians in long-term care in NewfoundlandLeader researcher: Shree Mulay |
|
Promising practice: Presence of family Our research focuses on long-term care (LTC) residents and family-centered care interventions – with the potential to change the way older adult care is provided in the province. Our aims include accelerating the availability of high-quality evidence to inform Canada’s rapid response to the COVID-19 pandemic; iterative testing to enhance local collaborative efforts and help reorient the existing research infrastructure; and providing evidence on older adults’ care for decision-making and planning throughout Canada. The interventions will include: e-visits and electronic messaging; virtual mental health support; residents’ integrated COVID and non-COVID care plans including virtual care; and infection control and prevention training among LTC leadership. Our findings will be relevant to all Canadian provinces with a population living in rural communities and small towns, and other settings that have similarities to those LTC homes in this province. |
Implementation of policies that support and hinder families as partners in care during the COVID-19 pandemic
Lead researcher: Janice Keefe
Host institution: Mount Saint Vincent University, Nova Scotia
Implementation of policies that support and hinder families as partners in care during the COVID-19 pandemicLead researcher: Janice Keefe |
|
Implementation of policies that support and hinder families as partners in care during the COVID-19 pandemic
Promising practice: Presence of family
Jurisdictions of focus: Digby, Sydney, Debert, Halifax (Nova Scotia), Charlottetown, Summerside (Prince Edward Island)
Prolonged separation from family members during the first wave of the COVID-19 pandemic had a huge negative impact on long-term care (LTC) residents’ well-being and quality of life. Family play a critical role in LTC, often helping with their loved one’s feeding, grooming and mobility. Our project focus is the implementation and sustainability of public health directives to increase the presence of family (and friends) in LTC homes through “support visitations” during the pandemic.
As public health restrictions fluctuate in response to the pandemic, it is important to understand the implementation process for support visitations, including how family has been engaged/represented; factors that support sustainability; and outcomes of support visitations for residents, family and staff.
Implementation of policies that support and hinder families as partners in care during the COVID-19 pandemicLead researcher: Janice Keefe |
|
Promising practice: Presence of family Prolonged separation from family members during the first wave of the COVID-19 pandemic had a huge negative impact on long-term care (LTC) residents’ well-being and quality of life. Family play a critical role in LTC, often helping with their loved one’s feeding, grooming and mobility. Our project focus is the implementation and sustainability of public health directives to increase the presence of family (and friends) in LTC homes through “support visitations” during the pandemic. As public health restrictions fluctuate in response to the pandemic, it is important to understand the implementation process for support visitations, including how family has been engaged/represented; factors that support sustainability; and outcomes of support visitations for residents, family and staff. |
Finding the right balance: implementing family presence policies in Ontario long-term care homes
Lead researcher: Samir Sinha
Host institution: Ryerson University, Ontario
Finding the right balance: implementing family presence policies in Ontario long-term care homesLead researcher: Samir Sinha |
|
Finding the right balance: implementing family presence policies in Ontario long-term care homes
Promising practice: Pandemic Response, Surge Capacity, Plan for COVID-19 and non-COVID-19 Care and Family Presence
Jurisdiction of focus: Toronto, Ottawa (Ontario)
The objective of this study was to examine how family presence policies can be better supported within long-term care homes to avoid residents sustaining severe and irreversible harms during COVID-19 and other pandemics.
The research team produced two key policy documents to provide long-term care homes, governments, and policy makers with timely, relevant and actionable evidence throughout the COVID-19 pandemic. They developed and published two guidance documents to support safe practices in long-term care homes during the pandemic.
The research team is producing a final policy document building on the previous two based on data collected with Hillel Lodge, a partner home.
The research team’s policy documents aim to put forth policies that balance long-term care resident safety and well-being and support safe visiting, in-home activities and outings. The documents released so far have enabled timely knowledge translation across sectors and fostered the use of high quality and real-time evidence by governments, policy makers and long-term care homes in the development and implementation of their re-opening policies. The research team continues to analyze the data gathered during this project to inform recommendations for next steps in long-term care.
Resources:
Finding the right balance: implementing family presence policies in Ontario long-term care homesLead researcher: Samir Sinha |
|
Promising practice: Pandemic Response, Surge Capacity, Plan for COVID-19 and non-COVID-19 Care and Family Presence Jurisdiction of focus: Toronto, Ottawa (Ontario) The objective of this study was to examine how family presence policies can be better supported within long-term care homes to avoid residents sustaining severe and irreversible harms during COVID-19 and other pandemics. The research team produced two key policy documents to provide long-term care homes, governments, and policy makers with timely, relevant and actionable evidence throughout the COVID-19 pandemic. They developed and published two guidance documents to support safe practices in long-term care homes during the pandemic. The research team is producing a final policy document building on the previous two based on data collected with Hillel Lodge, a partner home. The research team’s policy documents aim to put forth policies that balance long-term care resident safety and well-being and support safe visiting, in-home activities and outings. The documents released so far have enabled timely knowledge translation across sectors and fostered the use of high quality and real-time evidence by governments, policy makers and long-term care homes in the development and implementation of their re-opening policies. The research team continues to analyze the data gathered during this project to inform recommendations for next steps in long-term care. Resources: |
Dementia Isolation Toolkit Implementation Project
Lead researcher: Andrea Iaboni
Host institution: Toronto Rehabilitation Institute, Unity Health, Ontario
Dementia Isolation Toolkit Implementation ProjectLead researcher: Andrea Iaboni |
|
Dementia Isolation Toolkit Implementation Project
Promising practice: Prevention, people in the workforce, plan for COVID-19 and non-COVID-19 care and family presence
Jurisdiction of focus: Toronto, Petrolia, Sarnia (Ontario)
This research team partnered with three long-term care homes in Ontario to implement the Dementia Isolation Toolkit (DIT). The study aimed to:
- Co-design with key long-term care stakeholders including staff and family caregivers a customized DIT implementation protocol for each home.
- Improve the quality of care provided to residents in long-term care during isolation using the DIT.
- Measure the impact of the DIT on self-reported moral distress amongst long-term care homes.
- Identify factors (i.e., organizational culture, management, resources, or external policies) that influenced the adoption, use, and impact of the DIT on quality of care of residents and moral distress amongst staff.
Implementation of the DIT resulted in permanent, positive changes at two of three participating long-term care homes. Impacts include but are not limited to:
- The research team and partners learned how to approach the implementation of interventions in long-term care by adapting to the unique context, culture and needs of each home.
- The research team effected substantive changes to a long-term care home intake admission process with the goal of supporting a more person-centered transition and whole-person model of care.
- The research team co-designed and disseminated educational tools to support better communication and person-centered care in long-term care homes.
- The research team increased awareness of the signs and symptoms of moral distress in staff.
- Using input and evidence from this study, the research team developed a huddle to support communication and problem-solving around providing person-centered isolation care.
- The research team used their findings to advocate for changes to overcome system-level constraints to high quality, person-centered care.
Working conditions in long-term care impact the ability to promote change or improve the quality of resident care
The research team’s implementation of a person-centered care intervention during the pandemic was met with barriers that were often related to inadequate human resourcing, and challenging working conditions. Their experiences and findings working in long-term care support the notion that the conditions of work are the conditions of care and working conditions for staff will impact the quality of care they can provide residents, including their ability to engage with the DIT intervention.
Approaches to care planning in long-term care
Care planning in long-term care focuses on achieving minimum reportable standards of care (i.e., meeting basic physical needs of residents), versus a personalized and aspirational approach to set out a holistic plan of care to meet the physical, psychological, emotional, and social needs of residents living in long-term care. This research identified misalignment between the current standard approach to care planning and the approach to care planning that is supported by the DIT. Change in culture, values and the reportable standards of care that signal to long-term care staff what type of care is to be prioritized in long-term care settings is required to effect change.
Resources
Dementia Isolation Toolkit Implementation ProjectLead researcher: Andrea Iaboni |
|
Promising practice: Prevention, people in the workforce, plan for COVID-19 and non-COVID-19 care and family presence Jurisdiction of focus: Toronto, Petrolia, Sarnia (Ontario) This research team partnered with three long-term care homes in Ontario to implement the Dementia Isolation Toolkit (DIT). The study aimed to:
Implementation of the DIT resulted in permanent, positive changes at two of three participating long-term care homes. Impacts include but are not limited to:
Working conditions in long-term care impact the ability to promote change or improve the quality of resident careThe research team’s implementation of a person-centered care intervention during the pandemic was met with barriers that were often related to inadequate human resourcing, and challenging working conditions. Their experiences and findings working in long-term care support the notion that the conditions of work are the conditions of care and working conditions for staff will impact the quality of care they can provide residents, including their ability to engage with the DIT intervention. Approaches to care planning in long-term careCare planning in long-term care focuses on achieving minimum reportable standards of care (i.e., meeting basic physical needs of residents), versus a personalized and aspirational approach to set out a holistic plan of care to meet the physical, psychological, emotional, and social needs of residents living in long-term care. This research identified misalignment between the current standard approach to care planning and the approach to care planning that is supported by the DIT. Change in culture, values and the reportable standards of care that signal to long-term care staff what type of care is to be prioritized in long-term care settings is required to effect change. Resources |
Implementation of the “one high risk site only” policy
Lead researcher: Joanie Sims Gould
Host institution: University of British Columbia
Implementation of the “one high risk site only” policyLead researcher: Joanie Sims Gould |
|
Implementation of the “one high risk site only” policy
Promising practice: People in the workforce
Jurisdiction of focus: Vancouver, Richmond, Mission (British Columbia)
The objective of this research project was to evaluate the implementation and the impact of the one high risk site policy on long-term care homes, their staff, residents and their families.
The research team found that one high risk site policy had some unintended negative impacts on long-term care homes, their staff and residents.
The research highlighted the importance of developing and implementing policies in close collaboration with key long-term stakeholders including leaders, staff, residents and family representatives.
Implementation of the “one high risk site only” policyLead researcher: Joanie Sims Gould |
|
Promising practice: People in the workforce Jurisdiction of focus: Vancouver, Richmond, Mission (British Columbia) The objective of this research project was to evaluate the implementation and the impact of the one high risk site policy on long-term care homes, their staff, residents and their families. The research team found that one high risk site policy had some unintended negative impacts on long-term care homes, their staff and residents. The research highlighted the importance of developing and implementing policies in close collaboration with key long-term stakeholders including leaders, staff, residents and family representatives. |
Strengthening COVID-19 resilience of linguistic minorities in long-term care
Lead researcher: Idrissa Beogo
Host institution: Université de Saint-Boniface, Manitoba
Strengthening COVID-19 resilience of linguistic minorities in long-term careLead researcher: Idrissa Beogo |
|
Strengthening COVID-19 resilience of linguistic minorities in long-term care
Promising practices: Presence of family; prevention, people in the workforce
Jurisdictions of focus: Quebec City, Lameque (Quebec), Winnipeg, Sainte Anne (Manitoba), Moncton (New Brunswick)
In Canada, 81 percent of those who died in the first wave of COVID-19 lived in long-term care (LTC) homes. Reduced contact with professionals, families and caregivers arising from COVID-19 public health measures has led to unanticipated collateral effects – heightened isolation and loneliness for older adults, especially those belonging to minorities, and thus increased vulnerability.
In Quebec, a fifth of COVID-19 infections have involved healthcare workers. LTC homes are shorthanded, with exhausted staff afraid of infection. The vast majority have not optimally integrated computer technology. No one was prepared for the challenge of COVID-19, but innovations implemented so far have shown islands of success, and winning practices that our project will compile, with a focus on cultural-linguistic minorities.
Our project aims to identify and implement promising and best practices, create a community of practice to reduce isolation and loneliness in LTC residents, and ensure quality and safe care in LTC homes. Our focus is on older adults in linguistic and cultural minorities. Because of the very limited number of LTC homes dedicated to these populations, loved ones are often geographically distant, making digital solutions particularly useful.
Strengthening COVID-19 resilience of linguistic minorities in long-term careLead researcher: Idrissa Beogo |
|
Promising practices: Presence of family; prevention, people in the workforce In Canada, 81 percent of those who died in the first wave of COVID-19 lived in long-term care (LTC) homes. Reduced contact with professionals, families and caregivers arising from COVID-19 public health measures has led to unanticipated collateral effects – heightened isolation and loneliness for older adults, especially those belonging to minorities, and thus increased vulnerability. In Quebec, a fifth of COVID-19 infections have involved healthcare workers. LTC homes are shorthanded, with exhausted staff afraid of infection. The vast majority have not optimally integrated computer technology. No one was prepared for the challenge of COVID-19, but innovations implemented so far have shown islands of success, and winning practices that our project will compile, with a focus on cultural-linguistic minorities. Our project aims to identify and implement promising and best practices, create a community of practice to reduce isolation and loneliness in LTC residents, and ensure quality and safe care in LTC homes. Our focus is on older adults in linguistic and cultural minorities. Because of the very limited number of LTC homes dedicated to these populations, loved ones are often geographically distant, making digital solutions particularly useful. |
Supporting Mental Health and Preventing Moral Injury among Long Term Care Workers: A Mixed Methods Toolkit Implementation Study
Lead researcher: Bonnie Lashewicz
Host institution: University of Calgary, Alberta
Supporting Mental Health and Preventing Moral Injury among Long Term Care Workers: A Mixed Methods Toolkit Implementation StudyLead researcher: Bonnie Lashewicz |
|
Supporting Mental Health and Preventing Moral Injury among Long Term Care Workers: A Mixed Methods Toolkit Implementation Study
Promising practice: People in the workforce
Jurisdiction of focus: Edmonton, Calgary, Okotoks (Alberta)
This project investigated how to support the mental health and prevention of
moral injury among long-term care workers. The research aimed to:
- Gather stakeholder evidence about worker mental health needs and moral injury risks.
- Collect stakeholder assessments of a selection of mental health support/moral injury prevention tools.
- Create and disseminate a mental health support/moral injury prevention toolkit tailored to long-term care workers in pandemic conditions.
- Develop theory and evidence-based implementation strategies for scaling and spreading the toolkit.
The team is engaged in a continued research stream including an application to develop and test an employer-provided app to support long-term care workplace community-building and an application to examine policy obstacles and opportunities for increased employer-provided workplace community building tools.
Resources
Supporting Mental Health and Preventing Moral Injury among Long Term Care Workers: A Mixed Methods Toolkit Implementation StudyLead researcher: Bonnie Lashewicz |
|
Promising practice: People in the workforce Jurisdiction of focus: Edmonton, Calgary, Okotoks (Alberta) This project investigated how to support the mental health and prevention of moral injury among long-term care workers. The research aimed to:
The team is engaged in a continued research stream including an application to develop and test an employer-provided app to support long-term care workplace community-building and an application to examine policy obstacles and opportunities for increased employer-provided workplace community building tools. Resources |
Development and implementation of a clinical care pathway for frail older adults in long term care
Lead researcher: Zahra Goodarzi
Host institution: University of Calgary, Alberta
Development and implementation of a clinical care pathway for frail older adults in long term careLead researcher: Zahra Goodarzi |
|
Development and implementation of a clinical care pathway for frail older adults in long term care
Promising practice: Preparation and plan for COVID-19 and non-COVID-19 care
Jurisdiction of focus: Calgary (Alberta), Burnaby (British Columbia)
This research project aimed to develop an evidence-based care pathway for early recognition of frailty and initiation of early palliative care for long-term care residents, appropriate to the degree of frailty.
The research team’s objectives were to:
- develop an evidence-informed care pathway focused on diagnosing and managing frailty, including incorporating early palliative care in long-term care
- understand barriers and facilitators to this care pathway in long-term care
- develop and pilot an implementation strategy for the pathway.
Researchers conducted interviews and reviewed information available from long-term care homes to create the pathway. Despite difficulties with recruitment and availability during pandemic, the research team recruited a broad range of individuals in the Delphi procedure (a structured communication technique or method, originally developed as a systematic, interactive forecasting method which relies on a panel of experts) and have heard back from very interested individuals regarding creating a frailty care pathway. Multiple stakeholders from various different backgrounds provided feedback and were eager to help with this study. The Delphi resulted in a clinical pathway for frailty that we will base implementation on and is guided by experts in the field.
Relationships created from this study provided a path for researchers to better understand what long-term care homes are interested in implementing at their sites. Discussions with long-term care partners indicated that they are interested in implementing a frailty care pathway, addressing gaps in care related to frailty, and collaborating on future research to improve resident care. Implementing a clinical pathway for frailty in the long-term care sector can help better detect, treat and manage frailty in long-term care residents, appropriate to the degree of frailty, and encourage earlier access to palliative care. By creating a standardized pathway, healthcare teams can address residents’ needs better and improve or maintain their quality of life. Without a formal method of identifying frailty, later steps of management and treatment can be hindered. The research team will work with long-term care sites to implement the pathway to help provide earlier access to palliative care and frailty.
Development and implementation of a clinical care pathway for frail older adults in long term careLead researcher: Zahra Goodarzi |
|
Promising practice: Preparation and plan for COVID-19 and non-COVID-19 care Jurisdiction of focus: Calgary (Alberta), Burnaby (British Columbia) This research project aimed to develop an evidence-based care pathway for early recognition of frailty and initiation of early palliative care for long-term care residents, appropriate to the degree of frailty. The research team’s objectives were to:
Researchers conducted interviews and reviewed information available from long-term care homes to create the pathway. Despite difficulties with recruitment and availability during pandemic, the research team recruited a broad range of individuals in the Delphi procedure (a structured communication technique or method, originally developed as a systematic, interactive forecasting method which relies on a panel of experts) and have heard back from very interested individuals regarding creating a frailty care pathway. Multiple stakeholders from various different backgrounds provided feedback and were eager to help with this study. The Delphi resulted in a clinical pathway for frailty that we will base implementation on and is guided by experts in the field. Relationships created from this study provided a path for researchers to better understand what long-term care homes are interested in implementing at their sites. Discussions with long-term care partners indicated that they are interested in implementing a frailty care pathway, addressing gaps in care related to frailty, and collaborating on future research to improve resident care. Implementing a clinical pathway for frailty in the long-term care sector can help better detect, treat and manage frailty in long-term care residents, appropriate to the degree of frailty, and encourage earlier access to palliative care. By creating a standardized pathway, healthcare teams can address residents’ needs better and improve or maintain their quality of life. Without a formal method of identifying frailty, later steps of management and treatment can be hindered. The research team will work with long-term care sites to implement the pathway to help provide earlier access to palliative care and frailty. |
Preserving the link between cognitively impaired LTC residents and their families in the context of a pandemic: an evaluation of the implementation and effects of virtual and in-person interventions
Lead researcher: Marie-Soleil Hardy
Host institution: Université Laval, Quebec
Preserving the link between cognitively impaired LTC residents and their families in the context of a pandemic: an evaluation of the implementation and effects of virtual and in-person interventionsLead researcher: Marie-Soleil Hardy |
|
Preserving the link between cognitively impaired LTC residents and their families in the context of a pandemic: an evaluation of the implementation and effects of virtual and in-person interventions
Promising practice: Presence of family
Jurisdiction of focus: Saint-Jean-Port-Joli, Sainte-Marie, Thetford Mines, Saint-Augustin-de-Desmaures, Québec (Quebec)
The objective of this research project was to evaluate the implementation process, viability, and acceptability of interventions meant to privilege the presence of family, as well as the effects on residents, their caregivers, and the related costs. Through this work the research team addressed the experience and knowledge of users and their families, supported interventions to maintain contact between older adults with their loved ones and maximized and showcased the contribution of caregiver’s presence in older adults’ quality of life.
Introducing this innovation in long-term care homes created more opportunities to increase social connections by simply increasing the frequency of contact for caregivers who already had face-to-face visits or by providing the opportunity for potential caregivers living far away from the resident to have more visits with their loved ones.
Preserving the link between cognitively impaired LTC residents and their families in the context of a pandemic: an evaluation of the implementation and effects of virtual and in-person interventionsLead researcher: Marie-Soleil Hardy |
|
Promising practice: Presence of family Jurisdiction of focus: Saint-Jean-Port-Joli, Sainte-Marie, Thetford Mines, Saint-Augustin-de-Desmaures, Québec (Quebec) The objective of this research project was to evaluate the implementation process, viability, and acceptability of interventions meant to privilege the presence of family, as well as the effects on residents, their caregivers, and the related costs. Through this work the research team addressed the experience and knowledge of users and their families, supported interventions to maintain contact between older adults with their loved ones and maximized and showcased the contribution of caregiver’s presence in older adults’ quality of life. Introducing this innovation in long-term care homes created more opportunities to increase social connections by simply increasing the frequency of contact for caregivers who already had face-to-face visits or by providing the opportunity for potential caregivers living far away from the resident to have more visits with their loved ones. |
Making “non-essential” family/volunteer caregiving essential in long term care
Lead researcher: Annie Robitaille
Host institution: University of Ottawa, Ontario
Making “non-essential” family/volunteer caregiving essential in long term careLead researcher: Annie Robitaille |
|
Making “non-essential” family/volunteer caregiving essential in long term care
Promising practice: Presence of family, people in the workforce
Jurisdiction of focus: Ottawa, Welland, Vanier, Nepean (Ontario)
This research project aimed to:
- Gain a better understanding of the safety, efficacy, effectiveness, and ethics of COVID-19 policies that pertains to family presence in long-term care settings.
- Increase evidence on the impact of reduced levels of family/friend caregivers, formal volunteers, and staffing ratio due to COVID-19 on the short and anticipated long-term emotional and psychosocial well-being of residents, caregivers, and staff.
- Engage stakeholders in generating solutions and recommendations to revisit policies on family presence to improve current response and improve future pandemic and/or outbreak preparedness.
- Evaluate the implementation, adoption, effectiveness and sustainability of interventions and policies regarding family presence; and identify and address barriers and facilitators to the uptake of interventions and policy changes across settings.
The research team conducted 64 interviews with caregivers and volunteers supporting people living in long-term care and 20 interviews with residents. These interviews provided key lessons learned from the pandemic as it relates to the presence of care partners from the perspective of caregivers, volunteers, and long-term care home residents. The research team has also compiled suggestions for improvement and is gathering feedback from long-term care staff. The research team’s work improved understanding of how changes related to the pandemic impacted family members/caregivers, volunteers, and residents, the unique challenges faced as a result of reduced family/volunteer/caregiver levels and reduced contact with loved ones, knowledge about challenges and success stories and solutions for dealing with future pandemics and outbreaks.
This project has identified recommendations from the perspective of caregivers and long-term care home residents, and highlighted the importance of having researchers and knowledge users in long-term care work closely together.
Making “non-essential” family/volunteer caregiving essential in long term careLead researcher: Annie Robitaille |
|
Promising practice: Presence of family, people in the workforce Jurisdiction of focus: Ottawa, Welland, Vanier, Nepean (Ontario) This research project aimed to:
The research team conducted 64 interviews with caregivers and volunteers supporting people living in long-term care and 20 interviews with residents. These interviews provided key lessons learned from the pandemic as it relates to the presence of care partners from the perspective of caregivers, volunteers, and long-term care home residents. The research team has also compiled suggestions for improvement and is gathering feedback from long-term care staff. The research team’s work improved understanding of how changes related to the pandemic impacted family members/caregivers, volunteers, and residents, the unique challenges faced as a result of reduced family/volunteer/caregiver levels and reduced contact with loved ones, knowledge about challenges and success stories and solutions for dealing with future pandemics and outbreaks. This project has identified recommendations from the perspective of caregivers and long-term care home residents, and highlighted the importance of having researchers and knowledge users in long-term care work closely together. |
COVID-19: Implementation of virtual P.I.E.C.E.S™ for Resident Care Planning with Family to Build and Sustain Team Collaboration and Resilience for the Workforce in LTC Research Questions and Implementation Science Approach
Lead researcher: Denise Connelly
Host institution: Western University, Onatrio
COVID-19: Implementation of virtual P.I.E.C.E.S™ for Resident Care Planning with Family to Build and Sustain Team Collaboration and Resilience for the Workforce in LTC Research Questions and Implementation Science ApproachLead researcher: Denise Connelly |
|
COVID-19: Implementation of virtual P.I.E.C.E.S™ for Resident Care Planning with Family to Build and Sustain Team Collaboration and Resilience for the Workforce in LTC Research Questions and Implementation Science Approach
Promising practice: People in the workforce, family presence and plan for COVID-19 and non-COVID-19 care
Jurisdiction of focus: Chatham, Sarnia (Ontario)
This study sought to investigate the following research questions:
- What are lessons learned about enablers and challenges to implementation of a virtual P.I.E.C.E.S™ intervention for resident-centred care planning to prepare, support and guide the healthcare team (including resident/family/ staff) during COVID-19/flu outbreaks?
- Will implementation of a virtual P.I.E.C.E.S™ intervention help alleviate social isolation for residents, and improve family and team collaboration, leading to better outcomes for residents, resilience in registered practical nurses and communication between LTC homes and family?
Participant experiences suggest that implementation of registered practical nurse-led virtual P.I.E.C.E.S™ fostered individualized care, included family as partners in care, increased interdisciplinary collaboration and improved staff practices. Older adults and family/care partners perceived that they made valuable contributions to the research project. They were motivated to participate in the research project because they believed care delivery needed to be improved for older adults in long-term care with responsive behaviours. However, virtual P.I.E.C.E.S™, as delivered, lacked opportunities for family member feedback on older adult outcomes. Involving expert partners on the research team to bridge research and practice, developing relationships from a distance, empowering front-line champions, and adapting to challenging circumstances led to shared commitments for intervention success.
The research team observed that referrals to Behavioural Supports Ontario for behaviour support were reduced, suggesting that staff managed behaviour change cases very well; this is an important finding given statistics about increased use of antipsychotic medications in long-term care during the pandemic.
Lessons learned include the significance of stakeholder involvement throughout all research activities; the importance of clarity around expectations of all team members; and the consequence of readiness for implementation with respect to circumstances (e.g., COVID-19) and capacity for change.
Virtual engagement with family/care partners using the P.I.E.C.E.S™ care planning framework was preferred by staff and family/care partners with practice and improved skill in using virtual technology. To support sustainability and embedding virtual care planning as a best practice in long-term care homes, staff need to be engaged, supported to develop an algorithm that works for them, and trained and mentored to foster change for a culture of communication with older adults and their family/care partners for optimal care and joy in working in long-term care. The findings identified several recommendations for the long-term care sector including to:
- Strengthen technology infrastructure and knowledgeable use of technology in long-term care.
- Provide technology support for family/care partners and staff in long-term care.
- Identify research champions within long-term care homes to foster research engagement.
COVID-19: Implementation of virtual P.I.E.C.E.S™ for Resident Care Planning with Family to Build and Sustain Team Collaboration and Resilience for the Workforce in LTC Research Questions and Implementation Science ApproachLead researcher: Denise Connelly |
|
Promising practice: People in the workforce, family presence and plan for COVID-19 and non-COVID-19 care Jurisdiction of focus: Chatham, Sarnia (Ontario) This study sought to investigate the following research questions:
Participant experiences suggest that implementation of registered practical nurse-led virtual P.I.E.C.E.S™ fostered individualized care, included family as partners in care, increased interdisciplinary collaboration and improved staff practices. Older adults and family/care partners perceived that they made valuable contributions to the research project. They were motivated to participate in the research project because they believed care delivery needed to be improved for older adults in long-term care with responsive behaviours. However, virtual P.I.E.C.E.S™, as delivered, lacked opportunities for family member feedback on older adult outcomes. Involving expert partners on the research team to bridge research and practice, developing relationships from a distance, empowering front-line champions, and adapting to challenging circumstances led to shared commitments for intervention success. The research team observed that referrals to Behavioural Supports Ontario for behaviour support were reduced, suggesting that staff managed behaviour change cases very well; this is an important finding given statistics about increased use of antipsychotic medications in long-term care during the pandemic. Lessons learned include the significance of stakeholder involvement throughout all research activities; the importance of clarity around expectations of all team members; and the consequence of readiness for implementation with respect to circumstances (e.g., COVID-19) and capacity for change. Virtual engagement with family/care partners using the P.I.E.C.E.S™ care planning framework was preferred by staff and family/care partners with practice and improved skill in using virtual technology. To support sustainability and embedding virtual care planning as a best practice in long-term care homes, staff need to be engaged, supported to develop an algorithm that works for them, and trained and mentored to foster change for a culture of communication with older adults and their family/care partners for optimal care and joy in working in long-term care. The findings identified several recommendations for the long-term care sector including to:
|
Harnessing a novel partnership for COVID and non-COVID care in LTC
Lead researcher: Geetha Mukerji
Host institution: Women’s College Hospital, Ontario
Harnessing a novel partnership for COVID and non-COVID care in LTCLead researcher: Geetha Mukerji |
|
Harnessing a novel partnership for COVID and non-COVID care in LTC
Promising practice: Plan for COVID and non-COVID care
Jurisdiction of focus: Toronto (Ontario)
In the COVID-19 pandemic’s first wave, we developed and rapidly implemented a multi-institutional model of collaborative virtual care that provides long-term care (LTC) homes in the Greater Toronto Area with rapid access to specialists and diagnostic services. Our program, GTA-LTC+, initially focused on preventing avoidable hospital transfers, reflecting the perceived priority at the time. However, the need already existed pre-COVID-19 for more coordinated access to specialist care, ideally consolidated in a single partner hospital for any given LTC home.
GTA-LTC+ is useful in improving care even without the problems posed by COVID-19, with additional value in ensuring residents can continue to receive high quality, person-centered specialized care during future outbreaks. Our program uses a hub and spoke design, where six hospital hubs provide rapid access to a suite of virtual and in-person clinical and diagnostic services to geographically associated LTC homes in two of the five Ontario Health Regions (Toronto and Central).
Harnessing a novel partnership for COVID and non-COVID care in LTCLead researcher: Geetha Mukerji |
|
Promising practice: Plan for COVID and non-COVID care In the COVID-19 pandemic’s first wave, we developed and rapidly implemented a multi-institutional model of collaborative virtual care that provides long-term care (LTC) homes in the Greater Toronto Area with rapid access to specialists and diagnostic services. Our program, GTA-LTC+, initially focused on preventing avoidable hospital transfers, reflecting the perceived priority at the time. However, the need already existed pre-COVID-19 for more coordinated access to specialist care, ideally consolidated in a single partner hospital for any given LTC home. GTA-LTC+ is useful in improving care even without the problems posed by COVID-19, with additional value in ensuring residents can continue to receive high quality, person-centered specialized care during future outbreaks. Our program uses a hub and spoke design, where six hospital hubs provide rapid access to a suite of virtual and in-person clinical and diagnostic services to geographically associated LTC homes in two of the five Ontario Health Regions (Toronto and Central). |
Presence of Family and Other Informal Caregivers in Long-Term Care During COVID-19 and Beyond
Lead Researcher: Natasha Gallant
Host institution: University of Regina, Saskatchewan
Presence of Family and Other Informal Caregivers in Long-Term Care During COVID-19 and BeyondLead Researcher: Natasha Gallant |
|
Presence of Family and Other Informal Caregivers in Long-Term Care During COVID-19 and Beyond
Promising practice: Presence of family
Jurisdiction of focus: Saint John, NB and Hamilton, ON
With a focus on the presence of family, this research team co-developed interventions designed to support the presence of unpaid caregivers in long-term care homes during the COVID-19 pandemic.
This team developed a virtual course for unpaid caregivers requiring infection prevention and control training, established an online presence and a related advisory council focused on connecting residents and unpaid caregivers across Canada, and developed recommendations for integrating equity, diversity, and inclusion considerations in Canadian long-term care research.
Building on findings from this project, the research team is working with the Saskatchewan, Manitoba and New Brunswick governments and other relevant stakeholders to develop, implement and evaluate a social model of care that supports the mental health needs of residents and their unpaid caregivers.
Resources
Presence of Family and Other Informal Caregivers in Long-Term Care During COVID-19 and BeyondLead Researcher: Natasha Gallant |
|
Promising practice: Presence of family Jurisdiction of focus: Saint John, NB and Hamilton, ON With a focus on the presence of family, this research team co-developed interventions designed to support the presence of unpaid caregivers in long-term care homes during the COVID-19 pandemic. This team developed a virtual course for unpaid caregivers requiring infection prevention and control training, established an online presence and a related advisory council focused on connecting residents and unpaid caregivers across Canada, and developed recommendations for integrating equity, diversity, and inclusion considerations in Canadian long-term care research. Building on findings from this project, the research team is working with the Saskatchewan, Manitoba and New Brunswick governments and other relevant stakeholders to develop, implement and evaluate a social model of care that supports the mental health needs of residents and their unpaid caregivers. Resources |