Improving Equity in Access to Palliative Care Communities
Healthcare Excellence Canada and the Canadian Partnership Against Cancer are supporting 23 communities through the Improving Equity in Access to Palliative Care, a collaborative designed to make measurable improvement in access to palliative care with and for people experiencing homelessness or vulnerable housing.
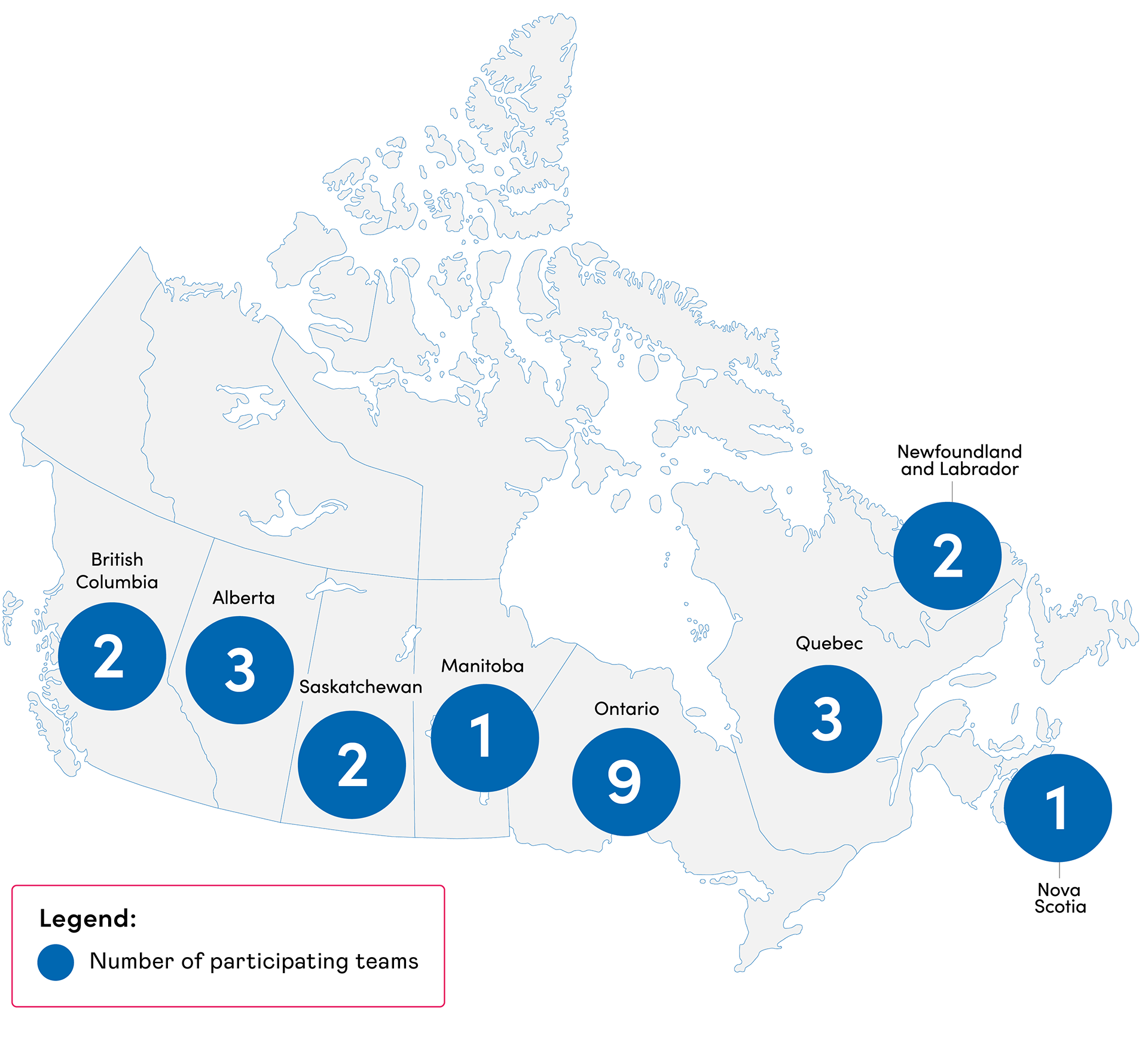
Alt text: A grey map of Canada with numerical values per province indicating the number of teams participating in the Improving Equity in Access to Palliative Care collaborative.
Featured content
From workshop to action: takeaways on equitable access to palliative care
In this blog, Improving Equity in Access to Palliative Care program coaches share takeaways from a health equity workshop, and the importance of improving access to palliative care with – and for – people experiencing homelessness.
Featured content
From workshop to action: takeaways on equitable access to palliative care
In this blog, Improving Equity in Access to Palliative Care program coaches share takeaways from a health equity workshop, and the importance of improving access to palliative care with – and for – people experiencing homelessness.
Participating communities and projects
The following teams have been accepted to participate in Improving Equity in Access to Palliative Care.
Alberta Health Services – North Zone (Bonnyville, Alberta)
Alberta Health Services is an integrated health authority that delivers health services provincially and is organized into five geographic zones – South, Calgary, Central, Edmonton and North. Provincewide supports are brought together strategically at the zone level to ensure integrated healthcare delivery that reflects unique local characteristics, from geography and history to culture. Alberta Health Services is partnering with Cold Lake First Nations Health Centre.
Through the collaborative, Alberta Health Services – North Zone aims to:
- Build capacity of care providers and community members to identify those who could benefit from a palliative approach to care that is culturally safe.
- Establish a sustainable care model extending services to individuals living on Cold Lake First Nation who wish to receive culturally safe palliative care within their community.
The Grey-Bruce Ontario Health Team (OHT) & Brightshores Health System (Grey Bruce Region, Ontario)
The Grey-Bruce OHT is a collective of care providers who work together to understand the unique healthcare needs of our communities, provide integrated healthcare services and improve healthcare delivery. Brightshores Health System operates six hospitals in the Grey Bruce region and offers a full range of specialty services.
The Grey Bruce OHT and Brightshores Health System is partnering with Saugeen First Nation, Chippewas of Nawash Unceded First Nation, Grey and Bruce Counties, Southwest Ontario Aboriginal Health Access Centre, Home and Community Care Support Services and the Grey Bruce Palliative Medicine Group to develop and deliver the Improving Equity in Access to Palliative Care collaborative.
In collaboration with local community partner organizations and people with lived and living experience, this project aims to:
- Build trust and develop meaningful relationships across our community.
- Increase capacity to offer a palliative approach to care for people experiencing homelessness or vulnerable housing as well as First Nations, Inuit and Métis who live on and off reserve.
- Improve access to high quality, dignified, culturally appropriate and equitable palliative care.
- Work with current services and providers to support referrals and deepen connections with priority population.
Champlain Hospice Palliative Care Program, Bruyère (Ottawa, Ontario)
The Champlain Hospice Palliative Care program (CHPCP) at Bruyère supports organizations that provide or wish to provide palliative care across the Champlain Region. The CHPCP works collaboratively with any organization that requests support to serve their clientele better and improve access to a palliative approach to care.
The CHPCP is partnering with Tungasuvvingat Inuit, Ottawa Inner City Health, The Ottawa Mission, Queen's University and the Division of Palliative Medicine at the University of Ottawa.
Through the collaborative, the CHPCP aims to:
- Understand the experiences of Inuit living with serious illness who seek or are eligible for palliative care in the urban setting of Ottawa and their opportunities to participate in decisions during this journey to receive palliative care.
- To tailor, apply and evaluate “Not Deciding Alone” in the context of palliative care. “Not Deciding Alone” is an Inuit-led project that community members have defined as supporting culturally safe care and consisting of tools and strategies for supporting clients in health decision-making.
- To engage in activities and practices, that community members define as culturally safe to support Inuit receiving palliative and end-of-life care.
Fort Erie Native Friendship Centre (Fort Erie, Ontario)
Fort Erie Native Friendship Centre (FENFC) Enhances All Aspects of Native Life while Extending Friendship to the Community. FENFC offers programming for all stages of life including family services, youth-based programs, lifelong care, employment and training to name a few. FENFC continues to expand and grow program and service offerings to match Community growth and identified needs. FENFC is honoured to partner with Hospice Niagara.
Through the collaborative, FENFC aims to:
- Create a sustainable volunteer peer-support program informed by an Indigenous approach to palliative care to better serve and improve access to palliative care for vulnerable people in the Fort Erie community.
Ongoing engagement with the Indigenous community will help to inform the direction of this initiative to ensure community needs are reflected in this model of care.
George Spady Society (Edmonton, Alberta)
The George Spady Society provides a continuum of support services to people with complex life circumstances associated with substance-related concurrent disorders and homelessness, empowering them to improve their lives through client-centred, evidence-informed best practices. The George Spady Society is partnering with the Palliative Care Outreach and Advocacy Team (PCOAT) at the Indigenous Wellness Clinic and the Calgary Allied Mobile Palliative Program (CAMPP).
Through the collaborative, the George Spady Society aims to:
- Provide palliative supports, home care, transitional support from acute to community care.
- Consult with healthcare providers and provide hospice support and information to people experiencing homelessness or vulnerable housing.
Huron Shores Family Health Team (Blind River, Ontario)
Huron Shores Family Health Team (HS FHT) is a not-for-profit healthcare organization that provides high-quality, interdisciplinary primary care and improves the health, well-being and quality of life for people in the communities of Blind River, Bruce Mines, Richards Landing and Thessalon. HS FHT is partnering with North Shore Health Network.
Through the collaborative, HS FHT aims to:
- Conduct a needs assessment to understand gaps and challenges in accessing care for people experiencing homelessness or vulnerable housing.
- Create a referral pathway and system navigation plan to address the palliative care needs of this population.
Institut de soins palliatifs et de fin de vie Michel-Sarrazin – Université Laval (Québec City, Québec)
The Institut de soins palliatifs et de fin de vie Michel-Sarrazin – Université Laval contributes to the field of palliative and end-of-life care through its research and knowledge transfer activities.
The Institut’s partners: Clinique SPOT; Direction du soutien à l’autonomie des personnes âgées, Centre intégré universitaire de santé et de services sociaux de la Capitale-Nationale; Lauberivière; Centre d’hébergement autochtone de Québec; Direction de la qualité, de l’évaluation, de l’éthique et des affaires institutionnelles, CHU de Québec; Ministère de la Santé et des Services sociaux, Direction des soins infirmiers et responsable du dossier des soins palliatifs.
Through the collaborative, the Institut de soins palliatifs et de fin de vie Michel-Sarrazin – Université Laval aims to forge ties between people who are homeless or at risk of homelessness, care providers, and community organizations in the Québec City region in order to adapt palliative and end-of-life care to the needs of homeless or precariously housed individuals.
Kingston Community Health Centres (Kingston, Ontario)
Kingston Community Health Centres is a dynamic provider of integrated services that empower people and build communities. They strive to create inclusive, resilient and healthy communities. Kingston Community Health Centres is partnering with Queen’s University Palliative Medicine Program, Home-Based Housing and Queen’s University.
Through the collaborative, Kingston Community Health Centres aims to better understand the unique needs of people experiencing homelessness or vulnerable housing and requiring palliative care services and ensure that they are connected to specialist palliative care services in a seamless and equitable manner.
Maison du Père (Montréal, Quebec)
Ever since it was founded in 1969, Maison du Père has been renowned for its innovative spirit and expertise with people experiencing homelessness. Over the years, the organization has offered clients a continuum of services including a prevention service, a shelter referral centre, a social reintegration and housing maintenance service, a residence for seniors on the street and a specialized and palliative health care wing for people without an address. Maison du Père is partnering with the Palliative Home-Care Society of Greater Montreal and the Fondation Virage, as well as several other partners.
Through the collaborative, Maison du Père aims to:
- Improve the experience of participants, their loved ones and providers by establishing a coordinated, user-friendly approach and integrating a harm-reduction approach for a broader client base.
- Strengthen collaboration and referrals between community, institutional and hospital partners.
- Improve access to care for clients experiencing homelessness in and around downtown Montréal, by increasing the number of spots available.
Medavie Health Services West - Moose Jaw (Moose Jaw, Saskatchewan)
Medavie Health Services West brings together four western emergency medical services (EMS) companies – MD Ambulance, Moose Jaw and District EMS, Guardian Ambulance, and Prairie EMS – into a single organization with regional expertise connected to national leadership in primary care. Medavie Health Services West - Moose Jaw is partnering with Square One Community Moose Jaw Inc., Thunder Creek Rehabilitation Association, Saskatchewan Health Authority and the Moose Jaw Age Friendly Committee.
Through the collaborative, Medavie Health Services West - Moose Jaw aims to provide medical supports and treatment, as well as referrals to appropriate resources, to people experiencing homelessness or vulnerable housing who have palliative care needs through their community paramedic program.
Newfoundland and Labrador (NL) Health Services – Labrador-Grenfell Zone (Nain, Newfoundland and Labrador)
NL Health Services provides a broad range of programs and services to the people of NL through a large suite of facilities, clinics, and community services, overseen by the health zones. The Labrador-Grenfell Zone serves all communities in Labrador, and those north of Barlett’s Harbour on the Northern Peninsula.
Through the collaborative, NL Health Services – Labrador-Grenfell Zone aims to implement a model of care through the Nain Community Clinic that enables community members to receive palliative care within their community and homes. This initiative is intended to reduce the number of individuals who must travel outside of their remote community to receive palliative care.
Newfoundland and Labrador (NL) Health Services – Eastern-Rural/Urban Zones (St. John’s, Newfoundland and Labrador)
As the provincial health authority, NL Health Services delivers high-quality health care to all residents of the province through a comprehensive range of programs. Utilizing an extensive network of facilities, clinics, and community services, we employ a zonal approach to ensure accessible and effective care for everyone.
The Eastern Urban Zone of NL Health Services, as part of the Downtown Health Collaborative, is partnering extensively with community organizations to improve health services and access to palliative and end of life care in the St. Johns Metro area.
Through the collaborative, NL Health Services – Eastern Zone aims implement a bed-based model of care within the community setting for people experiencing homelessness and unstable housing.
Niginan Housing Ventures (Edmonton, Alberta)
Niginan Housing Ventures is an Indigenous-led registered charity serving those hardest-to-house with complex medical, social and housing needs. They provide supportive, affordable housing opportunities for individuals and families who no other organization in Edmonton has successfully served. Residents are provided with loving and caring support for all areas of their lives and access to Indigenous ceremonies and cultural support.
Niginan Housing Ventures is partnering with Kokums Helper Society and other community partners such as George’s House.
Through the collaborative, Niginan Housing Ventures aims to:
- Provide Indigenous end-of-life care to the urban, houseless, vulnerable and predominantly Indigenous people.
- Create guidelines for Indigenous end-of-life care to support other communities to build capacity to deliver culturally safe(r) palliative care.
Nova Scotia Health (Central Zone, Nova Scotia)
Nova Scotia Health provides health services to Nova Scotians and some specialized services to Maritimers and Atlantic Canadians. It operates hospitals, health centres and community-based programs across the province. Nova Scotia Health is partnering with Northwood, the Victorian Order of Nurses and many other community partners to serve the most vulnerable.
Through the collaborative, Nova Scotia Health aims to:
- Develop a network of organizations and providers with the shared goal of improving equitable access to palliative care.
- Collaborate with community partners to adapt services to meet the needs of those experiencing homelessness or vulnerable housing by embedding services in local shelters and hospices.
- Build capacity across community partners to identify who may benefit from a palliative approach to care and what this approach looks like for this population.
Scarborough Centre for Healthy Communities/Inner City Health Associates (Scarborough, Ontario)
Scarborough Centre for Healthy Communities (SCHC) provides accessible, equitable and transformational health and social service choices for the well-being of diverse communities.
SCHC is partnering with Palliative Education and Care for the Homeless (PEACH), a program of the Inner City Health Associates (ICHA), to address a rapid increase in the number of Scarborough residents who have overlapping housing insecurity, marginalization and palliative care needs. PEACH is a partnership between ICHA, Toronto Centre Home and Community Care Support Services and Kensington Health.
Through the collaborative, SCHC aims to:
- Develop and implement a sustainable regional model of PEACH in Scarborough.
This model will be tailored to the unique needs of the Scarborough community.
The Palliative Home-Care Society of Greater Montreal (Montreal, Quebec)
The Palliative Home-Care Society of Greater Montreal enables all persons in the advanced stages of cancer or other life-limiting illnesses to conclude the final chapter of their lives in the comfort of their homes at no cost. From an academic and research perspective, the Society contributes to advancing knowledge in palliative care and participates in developing scientific and clinical approaches, particularly in-home palliative care. Through the program, the Society aims to:
- Strengthen partnerships with community-based organizations serving individuals experiencing structural vulnerabilities.
- Design and implement a sustainable outreach model that enables individuals living in a state of social precariousness to receive palliative care in the environment of their choice, thanks to the early referral of potential candidates.
- Develop resources to support reciprocal knowledge exchange within the community to better understand palliative approaches to care and the unique needs of people who are homeless or living in a state of precariousness.
The Dorothy Ley Hospice (Etobicoke, Ontario)
The Dorothy Ley Hospice is a volunteer-based community service organization offering compassionate care to people living with the challenges of a life-limiting illness or loss. Programs offered meet individual physical, emotional, spiritual and psychosocial needs to ensure each person can live life to the fullest. Through support from government donors and community partners, services are provided at no cost. The Hospice is partnering with GPS Health Navigators, Hope House Community Hospice and COMPASS Community Health Centre.
Through the collaborative, the Hospice aims to:
- Establish a system navigation service to ensure vulnerably housed refugees with Interim Federal Health Insurance and palliative care needs are connected with appropriate services.
- Increase awareness of insurance barriers for this population among community partners.
- Increase access to palliative care services for this population.
- This project will begin with a focus on communities including Mississauga, Hamilton and York Region, with opportunities to spread to other jurisdictions.
The Salvation Army Crossroads Residential Services (Saskatoon, Saskatchewan)
The Salvation Army Crossroads Residential Services, which opened in 1952, offers a Male-Identified Emergency Shelter program and the New Frontiers' Correctional Services Canada's halfway house program. Crossroads provides the Emergency After-Hours Program and a Community Feeding Program to support the vibrant community surrounding it. Crossroads is partnering with Medavie Health Services West.
Through the collaborative, Crossroads aims to:
- Embed paramedicine services focused on improving proximity to streamlined and dignified care within its shelter sites.
This initiative will involve the implementation of a health clinic informed by community needs.
Second Mile Club of Toronto/Kensington Health (Toronto, Ontario)
The Second Mile Club of Toronto/Kensington Health supports older adults and people living with disabilities in the community. They offer safe, recreational spaces and in-home services for older adults and adults living with disabilities. They also offer crisis intervention, home-making, senior active living centers, community day hospice and a caregiver support program.
The Second Mile Club of Toronto/Kensington Health is partnering with the PEACH – Palliative Education and Care for the Homeless program, which is a program through the Inner City Health Associates and The Neighborhood Group to ensure that the Peer Worker Initiative is collaborative and best serves the community we care for. The Second Mile Club of Toronto/Kensington Health is funded by the Ontario Ministry of Health, the Ontario Senior Secretariat, and the City of Toronto.
Through the collaborative, the Second Mile Club of Toronto/Kensington Health aims to provide support, advocacy and case management to individuals who are living with life-limiting illness while experiencing homelessness through a peer worker who will work alongside a health navigator.
Related resources:
- Palliative Education and Care for the Homeless (PEACH): A Model of Outreach Palliative Care for Structurally Vulnerable Populations (Healthcare Quarterly, April 2023): This article describes how PEACH’s unique model, critical community partnerships and research have been necessary for it to become a leader in community-based palliative care for structurally vulnerable people.
Thunder Bay Palliative Advocacy & Care Team (PACT) (Thunder Bay, Ontario)
Thunder Bay Palliative Advocacy & Care Team (PACT) provides primary healthcare and social services in the Thunder Bay community and surrounding District. PACT is partnering with Hospice Northwest, St. Joseph’s Group Northwest Regional Palliative Care Program, Thunder Bay Palliative Care Associates, the Centre for Education and Research on Acting and Health (CERAH) and NorWest Community Health Centre.
Through the collaborative, PACT aims to:
- Improve access to care through an outreach worker dedicated to vulnerably housed palliative care clients.
- Increase knowledge about palliative care among healthcare providers and people experiencing homelessness.
- Inform future programming though community engagement sessions and then build capacity to address identified needs in the community.
Vancouver Coastal Health/Providence Health Care (Vancouver, British Columbia)
Vancouver Coastal Health and Providence Health Care are responsible for the delivery of community, hospital and long-term care services to people in communities including Richmond, Vancouver, the North Shore, Sunshine Coast, Sea to Sky corridor, Powell River, Bella Bella and Bella Coola, and provide specialized care and services for people throughout the province.
Vancouver Coastal Health and Providence Health Care are the provincial hub for healthcare education and research, and together provide services to the Vancouver Downtown Eastside of Vancouver where a large community of people experience homelessness and/or precarious housing, and multiple other structural vulnerabilities.
Vancouver Coastal Health and Providence Health Care are partnering with Peer Operations/Overdose Emergency Response Team, Vancouver Coastal Health Indigenous Health, Vancouver Coastal Health Regional Mental Health/Substance Use, First Nations Health Authority, and BC Centre for Substance Use.
Through the collaborative, Vancouver Coastal Health and Providence Health Care aim to:
- Better understand the care planning preferences of patients who are experiencing homelessness or other structural vulnerabilities and living with a serious illness.
- Develop, implement and evaluate patient-informed best practice guidance for serious illness care planning conversations.
- Address barriers and improve communication and collaboration between teams that support patients in the Downtown Eastside community of Vancouver, including community care and acute care teams and other service providers.
Victoria Cool Aid Society (Victoria, British Columbia)
Victoria Cool Aid Society works with partners to offer life-changing services to adults impacted by poverty, colonization, stigma and homelessness. These services include permanent housing, emergency shelter, health and dental care, employment assistance, and social and recreational opportunities. Victoria Cool Aid Society is partnering with Island Health.
Building on foundational learnings from the Island Health’s Palliative Outreach Resource Team (PORT), the team is committed to meaningful community engagement and participatory action to develop a shared vision of palliative care services for the greater Victoria area.
Through the collaborative, the Victoria Cool Aid Society aims to:
- Co-design a sustainable model of care with community partners, including housing services, Island Health Authority, community-based care providers and people with lived and living experience.
- Implement and evaluate a community-based, end-of-life care environment (cluster of beds) for individuals experiencing homelessness or structural vulnerabilities in the greater Victoria area.
Winnipeg Regional Health Authority (Winnipeg, Manitoba)
The Winnipeg Regional Health Authority provides healthcare services to residents of the city of Winnipeg, as well as the northern community of Churchill and the rural municipalities of East and West St. Paul.
Winnipeg Regional Health Authority is partnering with George and Fay Yee Centre for Health Innovation and Shared Health to collaboratively work with existing partners who support those experiencing homelessness within the Winnipeg Health Region. Additional stakeholders and participating agencies will be added through an iterative, targeted engagement strategy as part of this collaborative.
Through the collaborative, the Winnipeg Regional Health Authority aims to establish and implement a strategic plan for providing palliative approaches to care for people experiencing homelessness or vulnerable housing within their jurisdiction.